Introduction to Acute Prostatitis
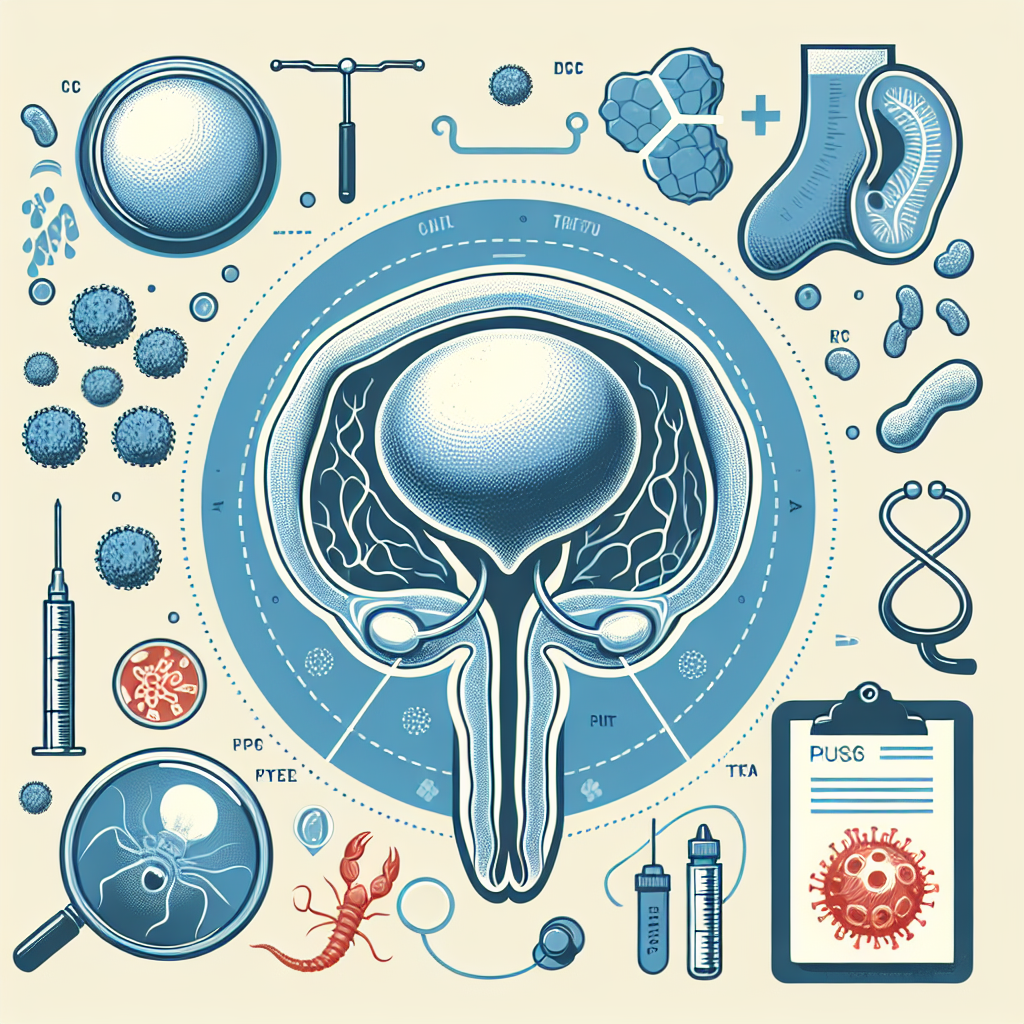
Acute prostatitis is a sudden and severe inflammation of the prostate gland, typically resulting from a bacterial infection. This condition necessitates immediate medical intervention, as it can lead to significant discomfort and serious complications if not addressed promptly. The bacteria responsible for this infection often travel to the prostate from the urinary tract or through the bloodstream. Common bacteria include Escherichia coli and other gram-negative organisms. This introduction sets the stage for understanding the severity and urgency associated with acute prostatitis, laying the groundwork for a detailed exploration of its pathology, diagnosis, symptoms, treatment, and complications in the subsequent sections of this article. The patient’s history, including any recent urinary tract infections or procedures involving the urinary tract, can provide critical clues in diagnosing acute prostatitis.
Common Symptoms of Acute Prostatitis
Acute prostatitis can manifest through a variety of symptoms, often presenting suddenly and with significant severity. Common symptoms include intense pelvic pain that can extend to the lower back and genital area. Patients frequently experience dysuria, marked by painful and difficult urination, along with an increased urinary frequency and urgency. In some cases, there may be visible blood or pus in the urine, indicating severe infection and inflammation. Additionally, systemic symptoms are often present, such as fever, chills, and general malaise, reflecting the body’s response to the infection. Acute prostatitis can also cause urinary retention due to swelling and inflammation obstructing the urethra. It’s essential for individuals exhibiting these symptoms to seek immediate medical attention to prevent further complications and to manage the condition effectively.
Diagnosis: How is Acute Prostatitis Identified?
Diagnosing acute prostatitis typically involves a combination of patient history, physical examination, and laboratory tests. Initial assessment often focuses on the sudden onset of symptoms such as high fever, chills, pelvic or rectal pain, and urinary issues. During the physical examination, a healthcare provider may perform a digital rectal exam (DRE) to evaluate the prostate gland. In the case of acute prostatitis, the prostate is often extremely tender, swollen, and warm to the touch. Laboratory tests play a crucial role in confirming the diagnosis and identifying the causative bacteria. A urine analysis and culture are commonly conducted to detect the presence of bacteria and white blood cells, signaling an active infection. Blood tests, including a complete blood count (CBC) and blood cultures, may also be performed to assess the severity of the infection and to check for bacteremia, a condition where bacteria enter the bloodstream. In certain situations, imaging tests such as an ultrasound or MRI might be recommended to rule out complications like abscesses or to provide a clearer view of the prostate and surrounding tissues. By combining these diagnostic approaches, healthcare professionals can accurately identify acute prostatitis and tailor appropriate treatment plans.
Primary Treatment Approaches for Acute Prostatitis
### Primary Treatment Approaches for Acute Prostatitis The primary treatment approaches for acute prostatitis focus on alleviating symptoms, eradicating the infection, and preventing complications. The standard treatment typically involves the use of antibiotics, given the bacterial origin of most cases. The choice of antibiotics is crucial and often starts with broad-spectrum antibiotics that target a wide range of bacteria, such as fluoroquinolones, until specific cultures can identify the causative agents. #### Antibiotic Therapy Antibiotic therapy remains the cornerstone of acute prostatitis treatment. Patients may initially be started on intravenous antibiotics, particularly if they present with severe symptoms, high fever, or are otherwise acutely ill. Once the patient stabilizes, the treatment can often transition to oral antibiotics, continued for several weeks to ensure thorough eradication of the infection. #### Pain Management Pain management is another critical aspect of treating acute prostatitis. Nonsteroidal anti-inflammatory drugs (NSAIDs) are frequently prescribed to reduce pain and inflammation. In cases of severe discomfort, stronger analgesics or even opioids might be considered. Additionally, alpha-blockers may be used to alleviate urinary symptoms by relaxing the muscles in the prostate and bladder neck, thus easing urination and reducing discomfort. #### Supportive Treatments Supportive treatments are also essential in managing acute prostatitis. Patients are encouraged to drink plenty of fluids to ensure adequate hydration and help flush bacteria from the urinary tract. Rest and avoidance of activities that exacerbate symptoms, such as heavy lifting or prolonged sitting, are recommended. #### Hospitalization In severe cases where patients exhibit significant systemic symptoms, such as high fever, chills, and an inability to urinate, hospitalization may be required. Inpatient care allows for close monitoring, intravenous fluids, and more aggressive management of symptoms and complications. #### Follow-Up Care Follow-up care is vital to ensure the infection has been fully resolved and to prevent recurrence. Patients typically undergo a repeat culture test to confirm the absence of bacteria and a physical examination to assess the resolution of symptoms. Regular follow-ups may be advised to monitor for any signs of chronic prostatitis or other complications. By adhering to these primary treatment approaches, healthcare providers can effectively manage acute prostatitis, alleviating symptoms and minimizing the risk of complications.
Potential Complications and How to Avoid Them
Acute prostatitis, if not treated properly and timely, can lead to several potential complications that may exacerbate the condition and affect the patient’s overall health. Some of the major complications include recurrent infections, chronic bacterial prostatitis, abscess formation, and systemic infections such as sepsis. Additionally, the inflammation can lead to urinary retention, bladder issues, and erectile dysfunction, significantly impacting the quality of life. To avoid these complications, it is crucial to follow the prescribed treatment regimen meticulously, complete the full course of antibiotics, and attend all follow-up appointments. Patients should also maintain a healthy lifestyle, stay hydrated, and practice good hygiene. Recognizing early symptoms and seeking prompt medical attention can prevent the escalation of the condition and reduce the risk of complications.
Understanding the Pathology Outlines
Understanding the pathology outlines of acute prostatitis is crucial for both healthcare professionals and patients. Pathology, in the context of acute prostatitis, refers to the study and diagnosis of the disease by examining tissues, cells, and other bodily fluids. The pathology outlines provide a systematic approach for identifying the underlying causes, assessing disease progression, and determining the appropriate treatment methods. One of the primary aspects of understanding pathology outlines is recognizing the characteristic features of acute prostatitis. This includes analyzing histopathological samples, which often reveal an infiltration of inflammatory cells, primarily neutrophils, in the prostate gland. The presence of bacterial colonies can also be detected in these samples, indicating the infectious nature of the condition. In addition to histopathological analysis, pathology outlines also encompass various diagnostic techniques such as urine tests, blood tests, and prostate-specific antigen (PSA) tests. Urine tests can help identify the presence of bacteria and white blood cells, suggesting an infection. Blood tests may show elevated white blood cell counts, further supporting the diagnosis of an acute infection. PSA tests can sometimes be elevated in acute prostatitis, although they are more commonly used for detecting prostate cancer. Understanding these pathology outlines is essential for accurate diagnosis and effective treatment planning. It helps in distinguishing acute prostatitis from other conditions with similar symptoms, such as chronic prostatitis or benign prostatic hyperplasia (BPH). Moreover, a clear understanding of the pathology of acute prostatitis enables healthcare providers to predict potential complications, such as abscess formation, sepsis, or chronic prostatitis, and to take appropriate preventive measures. In summary, the pathology outlines of acute prostatitis offer a comprehensive framework for understanding the disease at a micro-level. This knowledge is indispensable for accurate diagnosis, effective treatment, and prevention of complications, ultimately improving patient outcomes and quality of life.