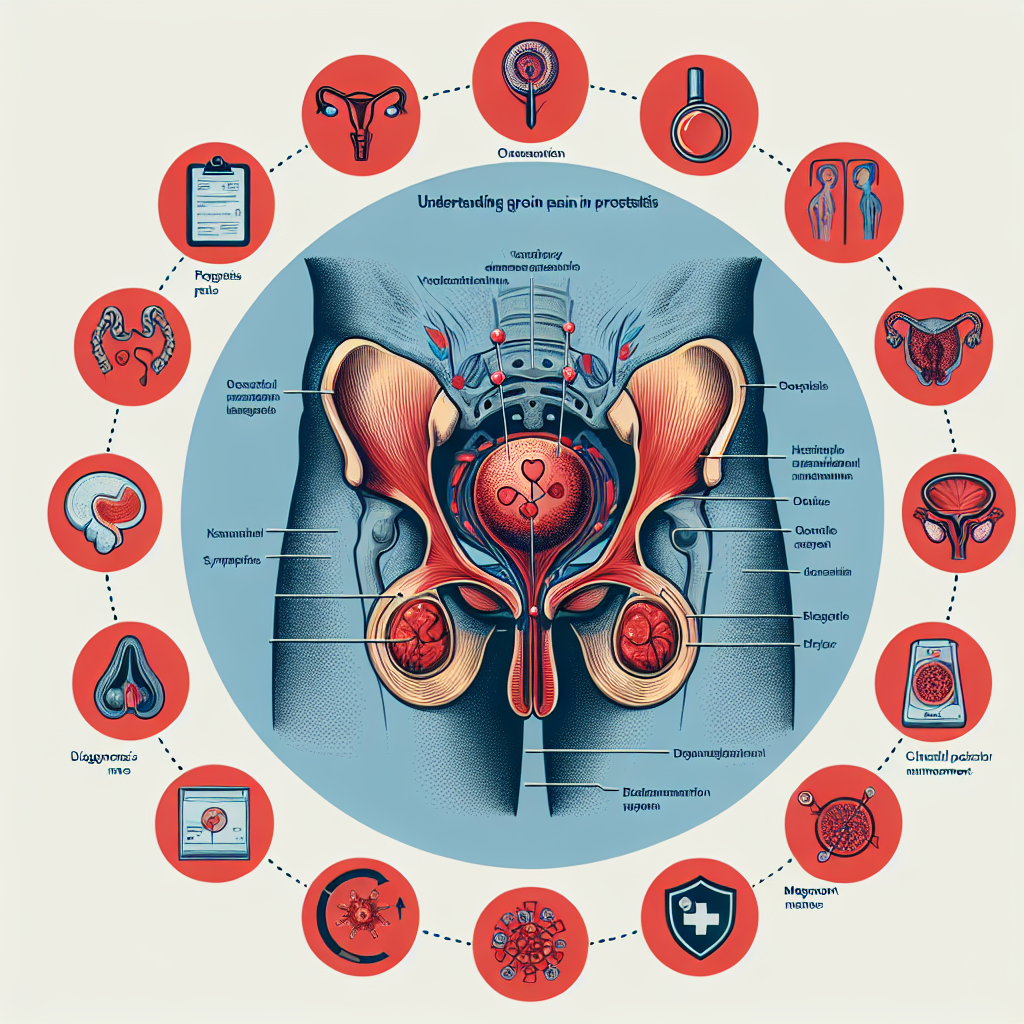
Symptoms and Diagnosis of Groin Pain in Prostatitis
Groin pain is a frequent symptom of prostatitis, an inflammation of the prostate gland that can result in a significant degree of discomfort and distress. The pain is typically strong, persistent, and localized in the groin area, which can extend to the lower abdomen, genital region, or even the lower back. It may worsen during physical activity or when seated for extended periods. Diagnosing groin pain associated with prostatitis involves a thorough medical history and physical examination. Physicians may perform digital rectal examinations (DRE) to assess the prostate gland’s size, shape, and tenderness. Additionally, diagnostic tests such as urinalysis, blood tests, prostate-specific antigen (PSA) tests, and imaging studies like ultrasound or MRI may be utilized to rule out other conditions and confirm the presence of prostatitis. Symptomatically, patients often report that the pain is accompanied by other manifestations such as urinary issues (frequent urination, urgency, and painful urination), sexual dysfunction (painful ejaculation and erectile difficulties), and general malaise (fever, chills, and fatigue). Recognizing the specific patterns of groin pain and these associated symptoms is essential for healthcare providers to make an accurate diagnosis and develop an effective treatment plan.
Types of Prostatitis and Their Symptoms
Trong phần này, chúng ta sẽ tìm hiểu về các loại viêm tuyến tiền liệt khác nhau và các triệu chứng liên quan đến chúng. ### Các Loại Viêm Tuyến Tiền Liệt Có nhiều loại viêm tuyến tiền liệt, mỗi loại có đặc điểm và biểu hiện riêng. Dưới đây là các loại chính. **Viêm Tuyến Tiền Liệt Cấp Tính Vi Khuẩn (Acute Bacterial Prostatitis):** Đây là loại viêm tuyến tiền liệt phổ biến và thường do vi khuẩn gây ra. Triệu chứng bao gồm sốt cao, ớn lạnh, khó tiểu, và đau ngực và lưng dưới. Đôi khi có thể kèm theo đau khi xuất tinh. **Viêm Tuyến Tiền Liệt Mãn Tính Vi Khuẩn (Chronic Bacterial Prostatitis):** Loại này có thể kéo dài nhiều tháng hoặc lâu hơn, và cũng do vi khuẩn gây nên. Triệu chứng thường nhẹ hơn so với viêm tuyến tiền liệt cấp tính, bao gồm đau vùng chậu, tiểu buốt, và đau khi quan hệ tình dục. **Viêm Tuyến Tiền Liệt Không Vi Khuẩn Mãn Tính (Chronic Nonbacterial Prostatitis):** Đây là loại viêm tuyến tiền liệt phổ biến nhất và không có liên quan đến nhiễm khuẩn. Triệu chứng thường bao gồm đau mãn tính ở vùng chậu, đau ngực, và rối loạn chức năng tiểu tiện. **Hội Chứng Đau Vùng Chậu (Chronic Pelvic Pain Syndrome – CPPS):** CPPS là một loại viêm tuyến tiền liệt mà nguyên nhân chưa được xác định rõ ràng. Triệu chứng bao gồm đau khi tiểu tiện, đau ở vùng sinh dục, và đau khi quan hệ tình dục. **Viêm Tuyến Tiền Liệt Không Triệu Chứng (Asymptomatic Inflammatory Prostatitis):** Loại này không gây triệu chứng rõ rệt và thường được phát hiện tình cờ qua các xét nghiệm khác. Mặc dù không gây khó chịu nhưng vẫn cần theo dõi và điều trị nếu cần thiết. Việc nhận biết và phân loại đúng loại viêm tuyến tiền liệt là vô cùng quan trọng để áp dụng phương pháp điều trị thích hợp.
Treatment Approaches for Groin Pain in Prostatitis
“Treatment Approaches for Groin Pain in Prostatitis”. Managing groin pain associated with prostatitis requires a multifaceted approach, addressing both the underlying infection or inflammation and alleviating the pain itself. Here, we explore various treatment modalities that have shown efficacy in treating groin pain in prostatitis sufferers.. Medical Treatments: One of the first lines of treatment involves the use of antibiotics for bacterial prostatitis. These medications can help to eliminate the infection causing the inflammation, thereby reducing pain. Non-bacterial prostatitis may require other types of medications like alpha-blockers, which help relax the muscle fibers in the prostate and bladder area, or anti-inflammatory drugs to reduce pain and swelling.. Physical Therapy: Physical therapy is another viable option, especially for those with chronic prostatitis. Techniques such as pelvic floor exercises can strengthen the muscles in the groin area, potentially alleviating pain. Biofeedback therapy and trigger point release are also alternatives frequently employed in chronic cases.. Lifestyle Changes: Lifestyle modifications are often recommended as an adjunct to medical treatment. These changes may include stress management techniques, dietary adjustments, and increased physical activity. Limiting caffeine, alcohol, and spicy foods can help minimize symptoms. Hydration is also crucial, as a well-hydrated body can better handle inflammation and pain.. Complementary Therapies: A growing number of patients report relief from complementary treatments. Acupuncture, chiropractic care, and herbal supplements may offer additional benefits. Though less scientifically established, these approaches can be combined with conventional treatments, provided they are discussed with a healthcare provider.. Psychological Support: Dealing with chronic pain can have a psychological toll. Cognitive-behavioral therapy (CBT) can help patients develop coping mechanisms and manage stress, which can in turn alleviate some of the physical symptoms. Support groups also offer an avenue for sharing experiences and finding communal support.. Each of these treatment options offers varying levels of relief, and what works for one individual may not work for another. Therefore, a tailored, comprehensive treatment plan developed in collaboration with healthcare providers is essential for effectively managing groin pain in prostatitis.
Managing Chronic Groin Pain in Prostatitis
Managing Chronic Groin Pain in Prostatitis can be a challenging aspect for many men who suffer from this condition. Groin pain, often persistent and debilitating, significantly impacts the quality of life and requires a comprehensive approach to treatment. Firstly, understanding the underlying causes of groin pain in prostatitis is crucial. It often arises due to the inflammation of the prostate gland, which can affect surrounding tissues and nerves, leading to discomfort and pain that may radiate to the groin area. Effective pain management strategies typically involve a combination of medications, physical therapy, lifestyle changes, and sometimes alternative therapies. Medications such as anti-inflammatories, pain relievers, and alpha-blockers can help reduce inflammation and alleviate pain. In some cases, antibiotics may be prescribed if a bacterial infection is present. Physical therapy is another vital component in managing chronic groin pain associated with prostatitis. A physical therapist can provide tailored exercises and stretches designed to reduce muscle tension and improve blood flow to the pelvic region, which may help alleviate pain. Techniques such as pelvic floor exercises, myofascial release, and biofeedback can be particularly beneficial. In addition to these conventional treatments, lifestyle modifications play an essential role in pain management. Stress management techniques, such as mindfulness and relaxation exercises, can help reduce overall tension and discomfort. Avoiding activities that exacerbate symptoms, maintaining a healthy diet, and staying hydrated are also critical in managing chronic groin pain. Furthermore, some patients may find relief through alternative therapies such as acupuncture, chiropractic care, or herbal supplements. While these approaches may not work for everyone, they can provide additional avenues for those seeking relief from chronic pain. It is important to discuss these options with a healthcare provider to ensure they are safe and appropriate for your specific condition. Overall, managing chronic groin pain in prostatitis involves a multifaceted approach that addresses both the physical and emotional aspects of the condition. By combining medical treatments with physical therapy, lifestyle changes, and possibly alternative therapies, patients can develop a comprehensive pain management plan that helps improve their quality of life.
Complications and Related Conditions
### Complications and Related Conditions Prostatitis, particularly when chronic, can lead to a host of complications and related conditions that may exacerbate the pain and discomfort experienced by the patient. One such complication is chronic pelvic pain syndrome (CPPS), which is characterized by prolonged pain and discomfort in the pelvic region, including the groin. This condition can significantly affect a patient’s quality of life, making daily activities and sexual function challenging. Another related condition is urinary tract infections (UTIs). The inflammation associated with prostatitis can cause bacteria to linger in the urinary tract, leading to recurrent infections. Symptoms of UTIs, such as a burning sensation during urination and frequent urges to urinate, can further aggravate groin pain and overall discomfort. Prostatitis can also influence sexual health. Erectile dysfunction (ED) and painful ejaculation are common among those suffering from this condition. The pain and psychological stress related to prostatitis can diminish sexual desire and performance, creating a vicious cycle that further hampers recovery. Moreover, some patients report issues with bowel movements, such as constipation or diarrhea. The proximity of the prostate to the lower digestive tract means that inflammation and pain can radiate to surrounding areas, compounding the discomfort. Lastly, untreated or poorly managed prostatitis can lead to mental health challenges, including anxiety and depression. Chronic pain, coupled with the social and intimate implications of this condition, can have a profound effect on mental well-being. Addressing these psychological components is crucial for comprehensive treatment and long-term management of prostatitis. Proper diagnosis and personalized treatment plans are essential to mitigate these complications and improve patient outcomes. Patients are encouraged to work closely with their healthcare providers to navigate the complexities of prostatitis and its related conditions.