Introduction to Granulomatous Prostatitis
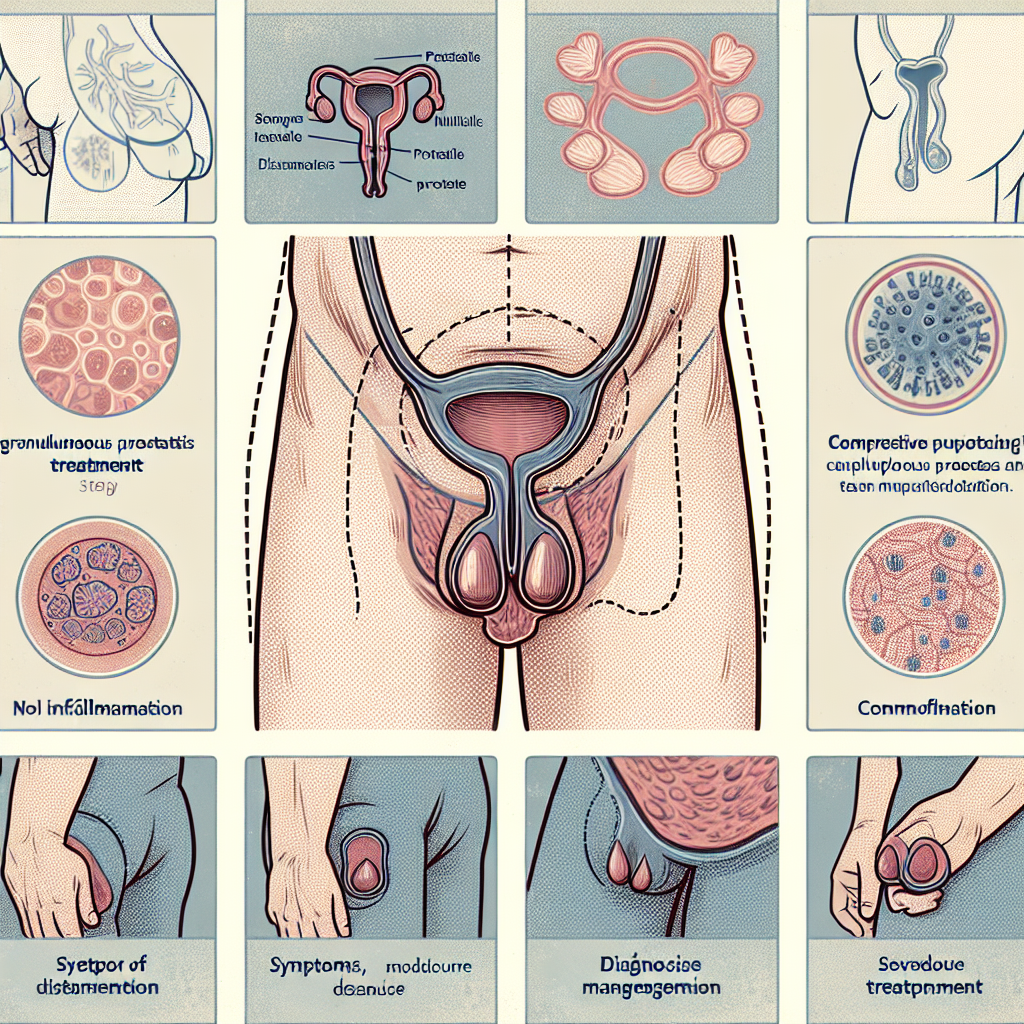
Granulomatous prostatitis, a specific subset of chronic prostatitis, is notably characterized by granuloma formations within the prostate gland. These granulomas consist of localized collections of immune cells which aggregate as a response to chronic inflammation. This condition, while rare, is significant due to its potential to mimic other more serious pathologies within the prostate, such as cancer. Understanding the nature of granulomatous prostatitis is the first step towards effective management. Patients often present with symptoms such as pelvic pain, urinary difficulties, and in some cases, asymptomatic inflammation detected during examinations for other conditions. Given the variable presentation, accurate diagnosis is crucial. Diagnosis typically involves a combination of laboratory tests, imaging studies, and histopathological examination through prostate biopsy. This comprehensive diagnostic approach helps to distinguish granulomatous prostatitis from other inflammatory or neoplastic prostate conditions. Within a pathological context, identifying the granulomatous formations can inform the medical team about the appropriate course of treatment. In this section, we will explore the pathophysiology of granulomatous prostatitis, its clinical manifestations, and the diagnostic challenges it presents. This foundational knowledge sets the stage for understanding the subsequent sections on management and treatment of this complex condition.
Symptoms and Diagnosis
### Symptoms and Diagnosis Granulomatous prostatitis often presents with a variety of symptoms that can overlap with other forms of prostatitis, making diagnosis challenging. Common symptoms include persistent pelvic pain, urinary discomfort, and increased urinary frequency. Some patients may also experience painful ejaculation and, in rare cases, blood in the urine or semen. Diagnosing granulomatous prostatitis typically begins with a thorough medical history and physical examination. Digital rectal examination (DRE) is an important first step, as it allows the healthcare provider to feel the prostate for abnormalities. If granulomatous prostatitis is suspected, further diagnostic tests are usually required to confirm the diagnosis. One of the primary diagnostic tools is transrectal ultrasound (TRUS), which helps visualize the prostate and identify areas of concern. Additionally, magnetic resonance imaging (MRI) can offer detailed imaging, further aiding in the diagnosis. Laboratory tests, such as urinalysis and prostate-specific antigen (PSA) levels, are also utilized but may not definitively indicate granulomatous prostatitis. A crucial component in confirming the diagnosis is a prostate biopsy. During this procedure, small tissue samples from the prostate are obtained and examined under a microscope. The presence of granulomas—small areas of inflammation composed of immune cells—directly supports the diagnosis of granulomatous prostatitis. In some instances, additional tests such as cystoscopy or uroflowmetry might be recommended to rule out other conditions or assess the severity of urinary symptoms. Given the complexity and rarity of granulomatous prostatitis, it is often diagnosed through a combination of clinical evaluation, imaging, and histological findings.
Conventional Treatment Methods
Conventional Treatment Methods Conventional treatment methods for granulomatous prostatitis primarily focus on alleviating symptoms and managing any underlying infections or inflammations. These treatments are typically the first line of defense and are often recommended due to their proven efficacy and accessibility. Here are some commonly used conventional treatment methods: 1. **Antibiotics:** If the granulomatous prostatitis is suspected to be caused by bacterial infections, antibiotics are often the prescribed treatment. These medications are aimed at eradicating the infection, thus reducing inflammation and discomfort. The choice of antibiotic and duration of treatment will depend on the type of bacteria cultured from the prostate or urine samples. 2. **Anti-inflammatory Medications:** Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or aspirin are commonly recommended to help manage pain and reduce inflammation associated with granulomatous prostatitis. Corticosteroids may also be prescribed in more severe cases to help control inflammation. 3. **Alpha Blockers:** Alpha blockers such as tamsulosin and alfuzosin can be used to relax the muscles in the prostate and bladder neck, which helps reduce urinary symptoms like difficulty in urination and frequent urge to urinate. These medications can significantly improve the quality of life for patients experiencing obstructive urinary symptoms. 4. **Pain Management:** In cases where pain is a significant concern, doctors may prescribe pain relief medication ranging from acetaminophen to stronger opioids, depending on the severity of the pain. Additionally, pelvic floor physical therapy might be recommended to help manage chronic pelvic pain. 5. **Surgical Intervention:** In some rare and severe cases where medications and other non-invasive treatments do not provide relief, surgical options may be considered. Procedures such as transurethral resection of the prostate (TURP) or other prostate surgeries might be recommended to remove granulomatous tissue and relieve symptoms. It’s important to consult a healthcare provider to determine the most suitable treatment plan based on the individual symptoms and severity of the condition. Conventional treatments are often tailored to the patient’s specific needs, making a personalized approach essential for effective management of granulomatous prostatitis.
Alternative Treatment Options
### Phương Pháp Điều Trị Thay Thế Trong khi thuốc và thay đổi lối sống là các lựa chọn điều trị chính cho viêm tuyến tiền liệt dạng hạt, một số bệnh nhân tìm kiếm các phương pháp điều trị thay thế nhằm bổ sung hoặc thay thế cho các phương pháp truyền thống. Các phương pháp này có thể giúp giảm triệu chứng, tăng cường sức khỏe tổng thể và nâng cao chất lượng cuộc sống. Dưới đây là một số phương pháp điều trị thay thế bạn có thể xem xét: 1. **Châm cứu:** Châm cứu là một liệu pháp truyền thống của Trung Quốc sử dụng kim nhỏ đâm vào các điểm cụ thể trên cơ thể để kích hoạt và cân bằng năng lượng. Một số nghiên cứu cho thấy châm cứu có thể giảm đau và cải thiện triệu chứng của viêm tuyến tiền liệt. 2. **Thảo dược:** Sử dụng các loại thảo dược có tính kháng viêm và kháng khuẩn đã được nhiều người tin dùng như là liệu pháp hỗ trợ. Nam việt quất, dầu cỏ Lúa mì và cây lưu ly đều là các loại thảo mộc nổi tiếng trong việc hỗ trợ sức khỏe tuyến tiền liệt. 3. **Liệu pháp xoa bóp tuyến tiền liệt:** Xoa bóp tuyến tiền liệt giúp cải thiện lưu thông máu và giảm sưng, đau. Tuy nhiên, lớp học về kỹ thuật đúng đắn là cần thiết để thực hiện phương pháp này một cách an toàn. 4. **Chế độ ăn uống:** Một chế độ ăn uống lành mạnh và cân bằng giàu chất chống ôi hóa có thể giúp cải thiện sức khỏe tuyến tiền liệt. Hãy tập trung vào các loại thực phẩm giàu omega-3, kẽm và lycopene như cá hồi, hạt bí, và cà chua. Hãy luôn tham khảo ý kiến bác sĩ trước khi bắt đầu bất kỳ phương pháp điều trị thay thế nào để đảm bảo chúng phù hợp với tình trạng cụ thể của bạn.
Lifestyle Changes and Management
Lifestyle changes play a significant role in managing granulomatous prostatitis and improving overall quality of life. Making deliberate adjustments to daily routines can help alleviate symptoms and prevent flare-ups. Here are some lifestyle modifications to consider: ## Diet and Nutrition A balanced diet rich in anti-inflammatory foods can aid in reducing inflammation in the prostate gland. Incorporate more fruits, vegetables, whole grains, and lean proteins into your meals. Omega-3 fatty acids, found in fish like salmon and flaxseeds, can also help in managing inflammation. It’s advisable to limit the intake of processed foods, saturated fats, and foods high in sugar, as these can exacerbate inflammation. ## Hydration Staying well-hydrated is essential for overall prostate health. Drinking plenty of water helps to flush out toxins and reduce the risk of urinary tract infections, which can complicate prostatitis. Aim for at least 8 glasses of water a day, and limit beverages that can irritate the bladder, such as caffeine and alcohol. ## Regular Exercise Engaging in regular physical activity can improve blood circulation and contribute to overall well-being. Low-impact exercises like walking, swimming, and cycling are particularly beneficial. Try to incorporate at least 30 minutes of moderate exercise into your daily routine. Additionally, pelvic floor exercises can strengthen the muscles around the prostate and improve urinary control. ## Stress Management Stress and anxiety can significantly impact the symptoms of granulomatous prostatitis. Practicing mindfulness techniques such as meditation, deep-breathing exercises, and yoga can help in managing stress levels. Consider setting aside time each day for relaxation and self-care activities that you enjoy. ## Smoking and Alcohol Both smoking and excessive alcohol consumption can aggravate symptoms of prostatitis. Quitting smoking and moderating alcohol intake are important steps in managing the condition. Seek support from healthcare professionals or support groups if you need assistance in making these changes. ## Sleep Hygiene Quality sleep is crucial for the body’s healing processes. Establish a regular sleep schedule, create a restful environment, and avoid screens before bedtime to improve sleep quality. Aim for 7-9 hours of sleep each night to support your overall health. By incorporating these lifestyle changes, individuals with granulomatous prostatitis can better manage their symptoms and enhance their quality of life. As always, it is important to consult with a healthcare provider before making any significant changes to your lifestyle or treatment plan.
Potential Complications
WP:Paragraph: While many individuals with granulomatous prostatitis can be effectively managed through a combination of medications, lifestyle changes, and alternative therapies, there are potential complications that may arise during the course of treatment. One of the main concerns is the risk of misdiagnosis, as granulomatous prostatitis can mimic other conditions such as prostate cancer or bacterial prostatitis. This can lead to unnecessary treatments or delays in appropriate care. Another complication is the potential for chronic pain and discomfort, which may persist even with treatment. Chronic prostatitis can also impact mental health, contributing to conditions such as depression and anxiety, particularly if symptoms are severe or persistent. Additionally, some treatment options might have side effects. For instance, long-term use of certain medications can lead to gastrointestinal issues, liver dysfunction, or cardiovascular problems. Patients should be closely monitored to mitigate these risks. Lastly, there is the possibility of recurrent infections or flare-ups, which can complicate the long-term management of the condition. Understanding these potential complications is essential for both patients and healthcare providers to develop a comprehensive and effective treatment plan.
Patient Stories and Experiences
Những câu chuyện và trải nghiệm của bệnh nhân Sự hiểu biết thực tế và tường thuật cá nhân từ những người đã trải qua viêm tuyến tiền liệt dạng hạt có thể cung cấp một góc nhìn rất khác so với những thông tin y tế thông thường. Những câu chuyện và trải nghiệm của bệnh nhân giúp làm sáng tỏ những khía cạnh của cuộc sống hàng ngày khi sống với tình trạng này, từ việc chẩn đoán ban đầu đến các phương pháp điều trị và quản lý triệu chứng. Một số bệnh nhân có thể chia sẻ rằng họ đã trải qua nhiều năm điều trị điều kiện này trước khi tìm ra phương pháp điều trị hiệu quả nhất cho mình. Chia sẻ những kinh nghiệm cá nhân này có thể mang lại hy vọng và sự thông cảm cho những người khác đang đối mặt với cùng một tình trạng. Những câu chuyện này không chỉ giúp việc hiểu sâu hơn về viêm tuyến tiền liệt dạng hạt mà còn tạo ra cảm giác cộng đồng và hỗ trợ giữa các bệnh nhân. Nhiều người có thể cảm thấy đơn độc trong cuộc chiến với bệnh lý này và việc nghe những câu chuyện của những người khác có thể mang lại sự động viên lớn lao.