Understanding Prostatitis and its Common Symptoms
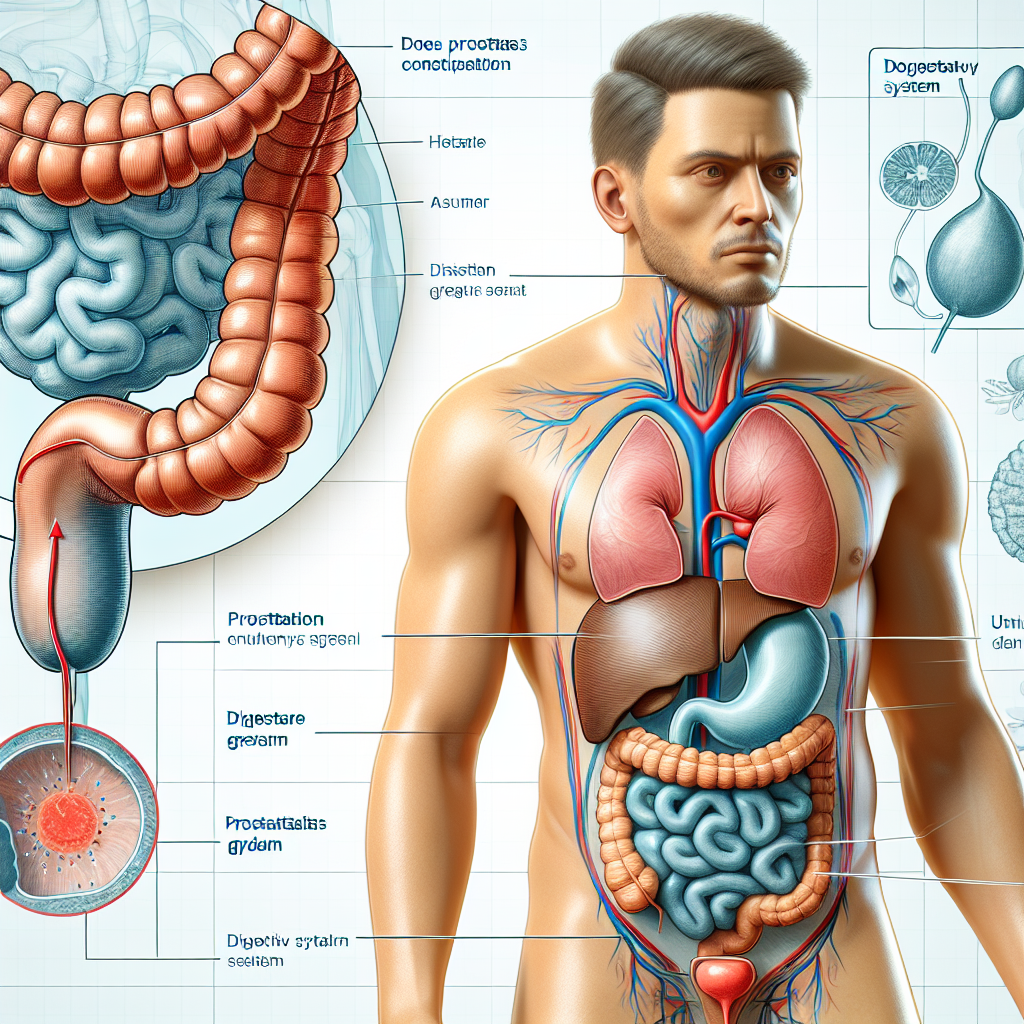
Prostatitis is a term that refers to inflammation of the prostate gland, a small gland that is part of the male reproductive system and is located just below the bladder. This condition can be classified into several types, including acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), and asymptomatic inflammatory prostatitis. Common symptoms of prostatitis can vary depending on the type but generally include pelvic pain, difficulty urinating, increased urinary frequency, painful urination, and sexual dysfunction such as painful ejaculation. In some severe cases, it can also lead to systemic symptoms like fever and chills. These symptoms can significantly impact a person’s quality of life and may require medical intervention to manage. One of the lesser-known symptoms that has been observed in some patients is constipation. While not as commonly discussed, constipation can co-occur with prostatitis, adding another layer of discomfort and complexity to the condition. The inflammation and swelling of the prostate can affect nearby organs and tissues, potentially leading to bowel symptoms. Understanding the interplay between the prostate gland and the digestive system is crucial for developing comprehensive treatment approaches that address all symptoms a patient may be experiencing.
The Anatomical Connection Between the Prostate and Digestive System
Mối Liên Kết Giải Phẫu Giữa Tuyến Tiền Liệt và Hệ Tiêu Hóa Trong lý do tìm hiểu cơ chế của cách mà viêm tuyến tiền liệt có thể gây ra táo bón, quan trọng là phải hiểu rõ mối liên hệ giải phẫu giữa tuyến tiền liệt và hệ tiêu hóa. Tuyến tiền liệt nằm ngay phía dưới bàng quang và trước trực tràng. Phần giữa của tuyến tiền liệt bao bọc quanh niệu đạo, ống dẫn nước tiểu từ bàng quang ra ngoài cơ thể. Các dây thần kinh và mạch máu kết nối tuyến tiền liệt với trực tràng có thể bị ảnh hưởng khi tuyến tiền liệt bị viêm. Sự viêm nhiễm này có thể tạo ra áp lực lên trực tràng, gây ra các triệu chứng khó chịu và ảnh hưởng đến chức năng tiêu hóa. Ngoài ra, viêm tuyến tiền liệt thường kết hợp với đau vùng chậu, mà có thể lan ra từ vùng bụng dưới và đùi trên. Những cơn đau này có thể làm suy yếu chức năng của cơ sàn chậu và cản trở việc nhu động ruột, dẫn đến tình trạng táo bón. Khi các cơ sàn chậu hoạt động không hiệu quả, khả năng tiêu hóa của cơ thể cũng bị ảnh hưởng. Điều này có thể làm chậm quá trình tiêu hóa, khiến phân không được vận chuyển dễ dàng qua đường ruột, gây ra táo bón. Hiểu rõ về mối liên hệ phức tạp giữa viêm tuyến tiền liệt và hệ tiêu hóa sẽ giúp trong việc xác định các biện pháp phòng ngừa và điều trị hiệu quả hơn cho bệnh nhân.
How Inflammation Can Influence Bowel Movements
Viêm đóng một vai trò quan trọng trong việc ảnh hưởng đến nhu động ruột. Khi cơ thể hưởng ứng viêm, các chất trung gian viêm như cytokine được sản xuất bởi hệ miễn dịch. Những chất này có thể tác động không chỉ đến khu vực viêm mà còn ảnh hưởng đến các cơ quan liên quan, bao gồm cả ruột. Trong trường hợp viêm tuyến tiền liệt, việc tiết ra các cytokine và các chất hóa học khác có thể tác động đến ruột, dẫn đến sự thay đổi trong nhu động ruột. Ngoài ra, viêm có thể kích thích các dây thần kinh và ảnh hưởng tiêu cực đến hệ thống tiêu hóa, gây ra tình trạng táo bón hoặc thay đổi thói quen đi tiêu. Hiểu được cách viêm ảnh hưởng đến nhu động ruột có thể giúp quản lý tốt hơn các triệu chứng liên quan và cải thiện chất lượng cuộc sống của bệnh nhân.
Symptoms and Diagnosis of Prostatitis-Related Constipation
Prostatitis, an inflammation of the prostate gland, can manifest a range of symptoms that vary in severity and impact on a patient’s daily life. One of the often-overlooked symptoms of prostatitis is constipation. Many healthcare providers and patients focus primarily on the more commonly discussed urinary and pelvic issues, but gastrointestinal symptoms can also be a significant concern. Constipation related to prostatitis is believed to arise from multiple factors. Firstly, the inflammation of the prostate can cause swelling and pressure on the surrounding tissues, including the rectum. This pressure can lead to discomfort and difficulty in passing stools. Patients may notice that they are unable to evacuate their bowels completely, leading to a sense of incomplete defecation. Additionally, prostatitis is often accompanied by pelvic pain and muscle spasms in the pelvic floor area. These spasms can affect bowel movements, making it more challenging for the body to coordinate the muscles necessary for a smooth passage of stools. The chronic pain associated with prostatitis can also contribute to a reluctance to strain during bowel movements, further exacerbating constipation. Diagnosing constipation related to prostatitis requires a comprehensive evaluation by a healthcare professional. A detailed medical history and physical examination are essential to rule out other potential causes of constipation. In some cases, additional tests such as a colonoscopy or imaging studies may be necessary to examine the structure of the colon and rectum. Healthcare providers often use a combination of symptom assessment tools and diagnostic criteria to identify constipation. These criteria typically include the frequency of bowel movements, stool consistency, and the presence of straining during defecation. Understanding the patient’s full range of symptoms, including urinary and gastrointestinal issues, is crucial for making an accurate diagnosis. Management of constipation in the context of prostatitis requires a multifaceted approach. Dietary changes, such as increasing fiber intake and staying hydrated, are foundational strategies. Physical therapy to strengthen the pelvic floor muscles can be beneficial, as can medications to manage inflammation and pain. In some instances, laxatives or stool softeners may be recommended to alleviate constipation temporarily while addressing the underlying prostatitis. Collaboration between urologists, gastroenterologists, and physical therapists can provide a comprehensive treatment plan tailored to the individual’s needs. By addressing both the prostatitis and constipation simultaneously, patients can achieve better overall health outcomes and improved quality of life.
Treatment Options for Managing Constipation Due to Prostatitis
When it comes to managing constipation caused by prostatitis, a multifaceted approach is often most effective. Both dietary adjustments and medical treatments may be required to alleviate symptoms. Here are some key treatment options to consider: 1. **Dietary Fiber and Hydration**: Increasing your intake of dietary fiber can help promote bowel regularity. Foods rich in fiber include fruits, vegetables, whole grains, and legumes. Additionally, staying well-hydrated by drinking plenty of water throughout the day can help soften stools and make them easier to pass. 2. **Probiotics**: Incorporating probiotics through supplements or fermented foods like yogurt and kefir can help maintain a healthy gut flora, potentially easing symptoms of constipation. 3. **Over-the-counter Remedies**: Various over-the-counter laxatives, such as bulk-forming agents, stool softeners, and osmotic laxatives, may provide short-term relief. However, it is crucial to consult your healthcare provider before using these products to ensure they are safe and appropriate for your specific condition. 4. **Prescription Medications**: In some cases, your doctor may prescribe medications specifically designed to treat constipation. These might include stronger laxatives or drugs that stimulate bowel movements. 5. **Physical Activity**: Regular physical activity can help enhance digestive function by stimulating intestinal activity. Aim to include moderate exercises such as walking, swimming, or cycling in your daily routine. 6. **Pelvic Floor Exercises**: Pelvic floor muscle training, also known as Kegel exercises, can help improve symptoms of prostatitis and may also benefit bowel function by strengthening the muscles involved in defecation. 7. **Stress Management**: Psychological stress can exacerbate both prostatitis and constipation. Techniques such as mindfulness meditation, deep breathing exercises, and cognitive-behavioral therapy (CBT) can be useful tools for managing stress. 8. **Consult a Specialist**: If your symptoms are severe or persistent, it may be beneficial to consult a gastroenterologist, a specialist in digestive health, who can perform additional tests and recommend more targeted treatments. By combining these various strategies, individuals suffering from constipation due to prostatitis can achieve better management of their symptoms and improve their overall quality of life. Always remember to consult your healthcare provider before initiating any new treatment regimen.
Lifestyle and Dietary Adjustments
Lifestyle and Dietary Adjustments When addressing the connection between prostatitis and constipation, a pivotal factor to consider is the role of lifestyle and dietary adjustments. Incorporating specific changes in daily habits can significantly improve both prostate health and digestive function. Healthy diet: Consuming a well-balanced diet rich in fiber is crucial. Fiber aids in softening stool and promoting regular bowel movements, which can help alleviate constipation. Include plenty of fruits, vegetables, whole grains, and legumes in your diet. Hydration: Proper hydration is essential for overall health and particularly important for maintaining digestive health. Drinking plenty of water can help prevent constipation by softening stool and promoting regular bowel movements. Exercise: Regular physical activity has numerous health benefits, including improving digestive function and reducing inflammation. Engaging in moderate exercise such as walking, swimming, or cycling can promote intestinal motility and help you stay regular. Stress Management: Stress can exacerbate both prostatitis and constipation. Techniques such as mindfulness meditation, deep breathing exercises, and yoga can help manage stress levels and improve overall well-being. Avoiding irritants: Certain foods and beverages can irritate the prostate and worsen symptoms of prostatitis. Limit intake of caffeine, alcohol, spicy foods, and acidic foods to help reduce inflammation and prevent digestive issues. Probiotic supplements: Probiotics can support a healthy gut microbiome and improve digestive health. Consider adding a probiotic supplement to your routine to help maintain regular bowel movements and support overall digestive function.
The Role of Medications and Prescriptions
The role of medications and prescriptions in managing prostatitis can significantly influence a patient’s overall digestive health, including the potential for experiencing constipation. Various medications are commonly prescribed to treat prostatitis, such as antibiotics for bacterial infections, alpha-blockers to relax the muscles in the prostate and bladder neck, and anti-inflammatory drugs to alleviate pain and swelling. While these medications can be effective in addressing the primary symptoms of prostatitis, they can also have side effects that impact the digestive system. Antibiotics, for example, are known to disrupt the natural balance of gut flora, potentially leading to gastrointestinal issues such as constipation. Similarly, alpha-blockers can cause relaxation in other muscle groups, including those in the gastrointestinal tract, which might slow down bowel movements. Patients managing prostatitis with medication should be aware of these potential side effects and discuss them with their healthcare provider. Working closely with a medical professional can help in adjusting dosages, switching medications, or incorporating supportive treatments like probiotics to maintain gut health. Ensuring a balanced approach to medication can mitigate the risk of constipation while effectively managing prostatitis symptoms. In addition to prescribed medications, lifestyle choices and over-the-counter remedies can also play a role in preventing or managing constipation. Increasing dietary fiber intake, staying hydrated, and engaging in regular physical activity can support healthy bowel movements and offset some of the constipation-inducing effects of medications prescribed for prostatitis.
When to Seek Medical Advice
When to Seek Medical Advice Dealing with prostatitis and its associated symptoms can be challenging, but knowing when to seek medical advice is crucial for effective management. If you experience persistent or severe symptoms, such as chronic pelvic pain, difficulty urinating, or significant constipation, it is essential to consult a healthcare professional. Additionally, if you notice any blood in your urine or semen, fever, or chills, you should seek immediate medical attention. A timely diagnosis can help prevent complications and provide you with a tailored treatment plan to alleviate your symptoms. Proactive medical care is key to maintaining both your prostate and digestive health.
Patient Experiences and Stories
Patient Experiences and Stories Patient experiences provide a valuable perspective on the relationship between prostatitis and constipation. Many individuals suffering from prostatitis have shared their personal struggles with constipation, adding a human element to clinical findings. For instance, John, a 45-year-old man diagnosed with chronic prostatitis, described his battle with severe constipation that coincided with flare-ups of his prostate symptoms. John’s story highlights how the discomfort and stress of prostatitis can exacerbate digestive issues. Similarly, Mark, a patient in his early 50s, noted that his constipation seemed to worsen during periods of heightened prostatitis symptoms. He emphasized the importance of a holistic treatment plan that addresses both prostate and digestive health. Mark found relief through dietary changes and pelvic floor exercises, which not only alleviated his constipation but also helped manage his prostatitis symptoms. These stories underscore the need for healthcare providers to consider the complex interplay between prostatitis and digestive health. Listening to patient experiences can guide more comprehensive and patient-centered approaches to treatment, ensuring that all aspects of a patient’s health are addressed. By sharing these narratives, we aim to provide hope and practical strategies for those struggling with the dual challenges of prostatitis and constipation.
Long-Term Management and Prevention
Trong quản lý lâu dài và phòng ngừa, việc duy trì một lối sống lành mạnh đóng vai trò cực kỳ quan trọng. Đối với nam giới bị viêm tuyến tiền liệt và mắc chứng táo bón, việc tiêu thụ đủ nước hằng ngày là vô cùng quan trọng. Nước có thể giúp hệ thống tiêu hóa hoạt động tốt hơn và giảm bớt triệu chứng táo bón. Cùng với lượng nước dồi dào, việc bổ sung nhiều chất xơ vào chế độ ăn uống cũng rất cần thiết. Chất xơ giúp tăng cường chức năng ruột và có thể là một phương pháp hiệu quả để ngăn ngừa táo bón dài hạn. Ngoài ra, việc thường xuyên tập thể dục không chỉ có lợi cho sức khỏe toàn diện mà còn có thể giúp giảm các triệu chứng về tiêu hóa. Các bài tập vận động nhàng nhàng như đi bộ, yoga hoặc bơi lội đều có lợi cho sức khỏe tuyến tiền liệt và hệ tiêu hóa. Một yếu tố không thể quên là việc kiểm tra sức khỏe định kỳ. Bạn nên thường xuyên tham khảo ý kiến của bác sỹ để có thể phát hiện sớm bất kỳ biến chứng nào và điều chỉnh phương pháp điều trị một cách hiệu quả nhất. Việc tránh xa các thói quen xấu như hút thuốc, uống rượu bia và ăn uống không lành mạnh cũng sẽ giảm thiểu nguy cơ viêm tuyến tiền liệt và các vấn đề về tiêu hóa. Cuối cùng, nếu bạn đang sử dụng thuốc hoặc các biện pháp điều trị khác, đừng quên hỏi ý kiến của chuyên gia về các tác dụng phụ có thể gây ra táo bón. Việc thay đổi liều lượng hoặc thay đổi loại thuốc có thể giúp giảm bớt tình trạng này.