Chronic Pain
Chronic pain is a frequent complication observed in individuals suffering from prostatitis and can significantly affect the quality of life. Unlike acute pain, which is usually temporary and directly related to tissue damage, chronic pain is persistent and can last for weeks, months, or even longer. This type of pain can be particularly challenging to manage, both for patients and healthcare providers. Living with chronic pain can lead to a myriad of other issues, including disturbed sleep, decreased appetite, and limited physical activity. It can also have a profound impact on mental health, increasing the risk of mood disorders such as depression and anxiety. The persistence of pain can lead to a sense of hopelessness and isolation, further exacerbating mental health problems. Managing chronic pain often requires a multifaceted approach. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics, and sometimes even antidepressants or anticonvulsants, may be prescribed to help alleviate the pain. Physical therapy can also be beneficial by improving mobility and reducing discomfort. Additionally, psychological support through counseling or therapy can be crucial in helping patients cope with the emotional toll of chronic pain. In some cases, alternative treatments such as acupuncture, biofeedback, or chiropractic care can provide relief for chronic pain sufferers. Lifestyle changes, including regular exercise, a balanced diet, and stress management techniques like meditation and yoga, can also be instrumental in managing chronic pain. Open communication between patients and healthcare providers is vital in the effective management of chronic pain. Patients should be encouraged to discuss the severity and impact of their pain openly, and healthcare providers should be prepared to offer a range of treatment options and support resources. Ensuring that patients have access to comprehensive pain management programs can significantly enhance their overall quality of life.
Urinary Problems
Vấn đề về đường tiểu là một trong những biến chứng phổ biến nhất liên quan đến viêm tuyến tiền liệt. Bệnh nhân thường trải qua các triệu chứng như cảm giác đau khi đi tiểu, đi tiểu nhiều lần, đặc biệt là vào ban đêm, cũng như cảm giác cần đi tiểu gấp nhưng không thể bắt buộc. Một số người có thể gặp khó khăn trong việc bắt đầu dòng chảy tiểu hoặc trải qua dòng chảy tiểu yếu, không đều. Những triệu chứng này không chỉ gây khó chịu mà còn ảnh hưởng đến chất lượng cuộc sống hàng ngày của bệnh nhân, gây ra căng thẳng và lo lắng về sức khỏe tổng thể của họ.
Sexual Dysfunction
Sexual dysfunction is one of the most distressing complications associated with prostatitis, posing a significant challenge to patients’ intimate relationships and overall emotional wellbeing. Sexual dysfunction can manifest in various forms, including erectile dysfunction, painful ejaculation, decreased libido, and difficulty achieving orgasm. These symptoms not only impede sexual satisfaction but can also lead to anxiety, depression, and a lowered sense of self-esteem, further exacerbating the psychological toll of prostatitis. A comprehensive approach to managing sexual dysfunction in prostatitis patients involves both medical and psychological interventions. Medically, doctors may prescribe medications that improve blood flow to the penis, such as phosphodiesterase type 5 inhibitors (e.g., sildenafil, tadalafil). Other treatments include alpha-blockers, which can relax muscle tissue in the prostate and bladder neck, alleviating some of the discomfort and potentially improving sexual function. In addition to pharmacological treatments, counseling and therapy play a vital role in addressing the emotional and psychological aspects of sexual dysfunction. Cognitive-behavioral therapy (CBT) can be particularly effective in helping patients manage anxiety and depression related to their sexual health. Furthermore, involving a partner in therapy sessions can improve communication and intimacy, fostering a supportive environment for both individuals. Pelvic floor physical therapy is another valuable tool, focusing on strengthening and relaxing the pelvic muscles. This kind of therapy can alleviate pain and improve blood flow, which is essential for maintaining erectile function and enhancing sexual pleasure. Lifestyle modifications, such as regular exercise, a healthy diet, and quitting smoking or excessive alcohol consumption, can also have a positive impact on sexual health. Managing sexual dysfunction in the context of prostatitis requires a holistic approach that addresses both the physical symptoms and the emotional consequences of the condition. By integrating medical treatments, psychological support, and lifestyle changes, patients can experience significant improvements in their sexual health and overall quality of life.
Emotional and Psychological Impact
Prostatitis không chỉ gây ảnh hưởng đến sức khỏe thể chất mà còn có thể gây ra những tác động nghiêm trọng đến tâm lý và cảm xúc của người bệnh. Quá trình xử lý một tình trạng sức khỏe mãn tính như viêm tiền liệt tuyến thường đi kèm với sự lo âu, căng thẳng và có khi là tình trạng trầm cảm. Một trong những yếu tố tác động mạnh mẽ đến tâm lý của người bệnh chính là sự đau đớn và khó chịu kéo dài. Cảm giác đau rát, đặc biệt là ở vùng hạ tầng, có thể gây ra tình trạng mất ngủ, thay đổi tâm trạng và giảm khả năng thực hiện các hoạt động hàng ngày. Một cảm giác bức bối, không thoải mái luôn tồn tại có thể khiến người bệnh cảm thấy bị cô lập và dễ nổi cáu. Ngoài ra, chứng mất tình dục và suy giảm chất lượng cuộc sống tình dục cũng là một nguồn gốc quan trọng gây ra stress tâm lý. Sự lo âu và những áp lực về sự nam tính, khả năng duy trì một mối quan hệ tình cảm và hạnh phúc gia đình đều bị thách thức khi chức năng sinh dục bị ảnh hưởng. Sự thiếu hiểu biết về bệnh tình và cảm giác bất lực trong việc kiểm soát triệu chứng cũng tăng cường cảm giác lo lắng. Sự không chắc chắn về liệu trình điều trị hiệu quả và thời gian hồi phục kéo dài có thể gây ra những suy nghĩ tiêu cực và tinh thần bi quan. Để quản lý những tác động tâm lý và cảm xúc này, việc hỗ trợ tâm lý đóng vai trò quan trọng. Các phương pháp tiếp cận như liệu pháp hành vi nhận thức (CBT) có thể giúp người bệnh học cách điều chỉnh suy nghĩ tiêu cực và phản ứng một cách tích cực hơn. Ngoài ra, việc giao tiếp cởi mở với gia đình, bạn bè và các nhóm hỗ trợ cũng rất cần thiết để giúp người bệnh cảm thấy được sự ủng hộ và giảm bớt tình trạng cô lập. Chăm sóc sức khỏe tâm lý không nên bị xem nhẹ khi xử lý viêm tiền liệt tuyến. Tích hợp các phương pháp hỗ trợ tâm lý vào kế hoạch điều trị tổng thể có thể giúp nâng cao chất lượng cuộc sống tổng thể cho người mắc bệnh, đồng thời giúp họ cảm thấy vững tâm hơn trong quá trình hồi phục.
Increased Risk of Other Conditions
wp:paragraph Increased Risk of Other Conditions Patients suffering from prostatitis are at a heightened risk of developing other health conditions, which can further complicate their overall wellbeing. One such condition is chronic pelvic pain syndrome (CPPS), a leading cause of persistent pain and discomfort in the pelvic region. CPPS is often linked to prostatitis and can significantly diminish a patient’s quality of life, making daily activities challenging. Additionally, men with prostatitis may face an elevated risk of urinary tract infections (UTIs). UTIs can cause severe discomfort, frequent urination, and pain, requiring ongoing medical treatment and management. This correlation between prostatitis and UTIs highlights the importance of vigilant monitoring and timely intervention. Moreover, inflammation associated with prostatitis can sometimes lead to issues with sexual function, including erectile dysfunction (ED) and painful ejaculation. Such complications can have profound psychological effects, contributing to stress, anxiety, and depression among sufferers. Lastly, there is a potential risk of infertility linked to chronic prostatitis. The inflammation and bacterial infections adversely affect the prostate and surrounding structures, interfering with their normal functioning. Men dealing with symptoms of prostatitis should be aware of these interconnected risks and work closely with healthcare providers to manage and mitigate these complications effectively. /wp:paragraph
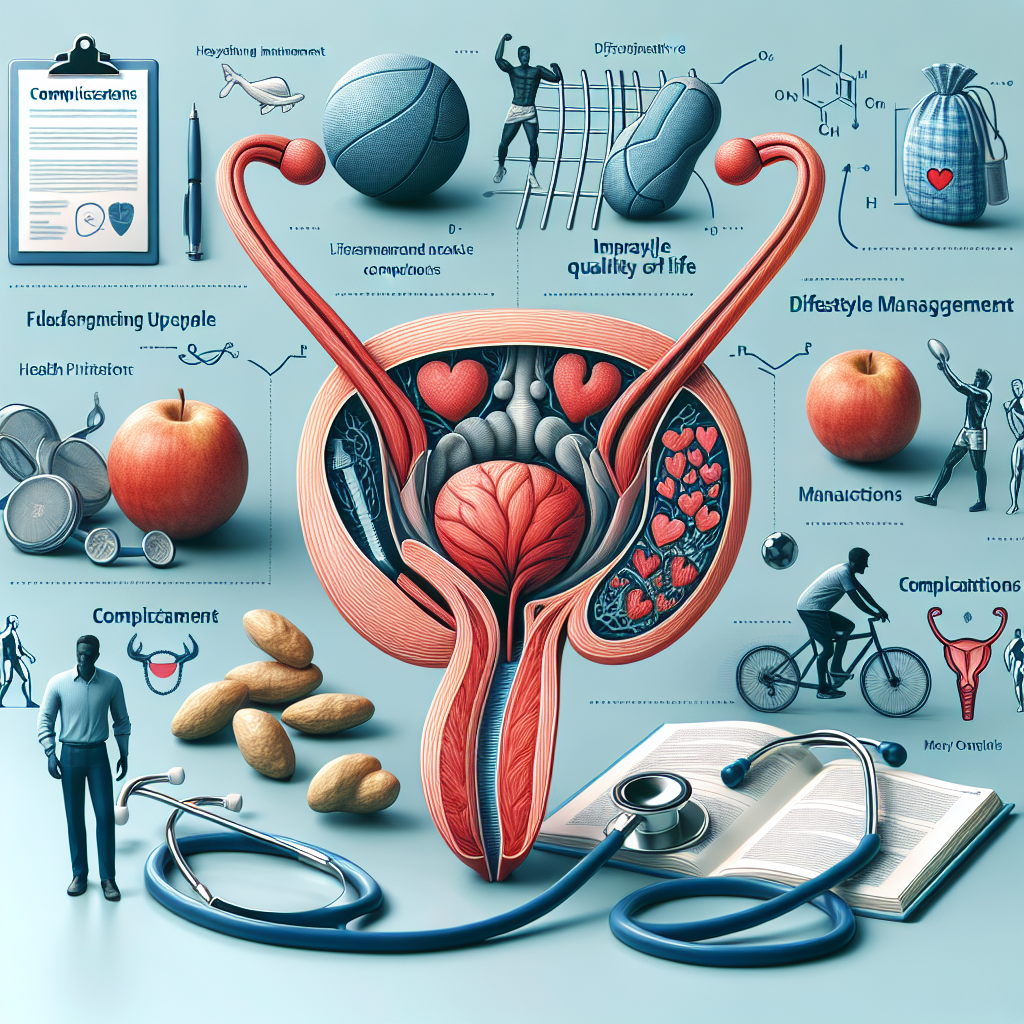
Management Strategies
Effective management strategies for prostatitis complications are essential for improving patient outcomes and quality of life. One of the primary approaches involves medication management, which can include antibiotics for bacterial prostatitis, alpha-blockers to relieve urinary symptoms, and anti-inflammatory drugs to reduce pain and swelling. Alongside pharmaceuticals, patients are often guided to adopt lifestyle modifications such as increasing fluid intake, avoiding irritants like caffeine and alcohol, and practicing regular physical activity to support overall health. Another vital aspect is the incorporation of pelvic floor exercises, which can strengthen the muscles supporting the bladder and prostate, thereby alleviating symptoms. Collaborative care involving multidisciplinary teams, including urologists, physical therapists, and mental health professionals, ensures a comprehensive approach to managing not just the physical, but also the emotional and psychological impacts of prostatitis. Regular follow-up and monitoring, patient education, and support groups play a crucial role in maintaining adherence to treatment plans, managing stress, and providing coping mechanisms. By employing a variety of management strategies, patients with prostatitis can achieve significant improvements in their quality of life despite the challenges posed by the condition.