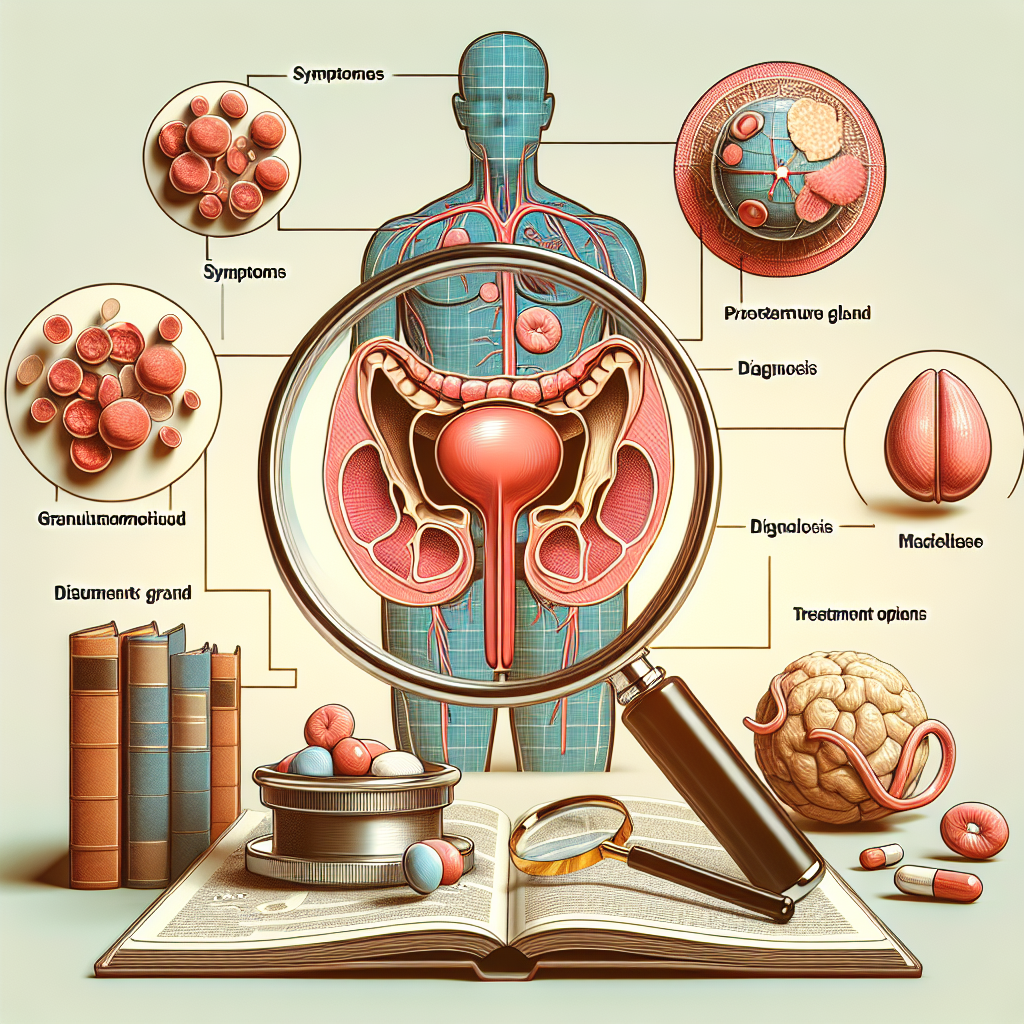
What is Granulomatous Prostatitis?
Granulomatous prostatitis is an uncommon inflammatory condition characterized by the presence of granulomas in the prostate gland. Granulomas are collections of immune cells that form in response to chronic inflammation or infection, and they can lead to tissue damage and scarring. This condition can be classified into several subtypes, including infectious granulomatous prostatitis, idiopathic granulomatous prostatitis, and iatrogenic granulomatous prostatitis. Each subtype has distinct underlying causes, ranging from bacterial and fungal infections to surgical procedures and medical interventions. The precise cause of idiopathic granulomatous prostatitis remains unknown. Due to its rarity and the potential for significant overlap in clinical, radiologic, and histologic features, granulomatous prostatitis can be difficult to diagnose. Common symptoms include pelvic pain, urinary frequency and urgency, painful urination, and blood in the urine or semen. These symptoms are often nonspecific, making it easy to mistake this condition for other types of prostatitis or even prostate cancer. As a result, thorough diagnostic evaluation is essential for accurate identification. Diagnostic methods may include digital rectal examination, prostate-specific antigen (PSA) testing, imaging studies such as ultrasound or MRI, and prostate biopsy. Histopathologic analysis of biopsy samples is critical for confirming the presence of granulomas and ruling out malignancy. Understanding the unique characteristics of granulomatous prostatitis is crucial for selecting appropriate treatment options. Therapeutic approaches may vary depending on the underlying cause and the severity of symptoms. Treatment options can include antibiotics for infectious causes, corticosteroids to reduce inflammation, and other immunosuppressive medications for autoimmune forms of the condition. In some cases, surgical intervention may be necessary to remove obstructive or severely damaged tissue. Ongoing research and advances in medical science continue to improve our understanding of granulomatous prostatitis, offering hope for more effective management strategies in the future.
Symptoms of Granulomatous Prostatitis
Những triệu chứng của viêm tuyến tiền liệt dạng hạt có thể rất đa dạng và thường trùng lặp với các loại viêm tuyến tiền liệt khác, làm cho việc chẩn đoán trở nên khó khăn. Một trong những triệu chứng phổ biến nhất là đau ở vùng đáy chậu, tầng sinh môn hoặc vùng dưới hông. Bệnh nhân cũng có thể cảm thấy khó tiểu, bao gồm tiểu khó, tiểu đau hoặc cảm giác tiểu không hoàn toàn. Một số người có thể gặp triệu chứng như sốt hoặc ớn lạnh, do viêm nhiễm cấp tính kèm theo. Trong nhiều trường hợp, bệnh nhân có thể cảm thấy đau ở vùng bụng dưới hoặc vùng chậu, cũng như cảm giác muốn đi tiểu thường xuyên nhưng không tiểu hết được. Một số trường hợp nặng có thể xuất hiện máu trong tinh dịch hoặc nước tiểu, điều này có thể gây lo ngại và cần được khám sàng lọc bệnh chủ động. Không phải tất cả các triệu chứng đều xuất hiện đồng thời ở mọi bệnh nhân, điều này làm cho việc xác định viêm tuyến tiền liệt dạng hạt trở nên phức tạp hơn. Vì vậy, nếu có bất kỳ triệu chứng nào kể trên, bệnh nhân nên tìm kiếm lời khuyên từ các chuyên gia y tế để được chẩn đoán và điều trị kịp thời. Xét nghiệm và siêu âm có thể giúp xác định chính xác tình trạng và sự hiện diện của các nốt hạt trong tuyến tiền liệt.
Causes and Risk Factors
Causes and Risk Factors The precise causes of granulomatous prostatitis are not always clear, but various factors can contribute to its development. One common cause is an autoimmune response, where the body’s immune system mistakenly attacks healthy prostate tissue, leading to inflammation and granuloma formation. This type of autoimmune response may be triggered by infections, injuries, or other underlying conditions. Infectious agents, such as bacteria, fungi, and viruses, can also play a significant role in the onset of granulomatous prostatitis. For instance, bacterial infections like tuberculosis or fungal infections can cause granulomatous changes in the prostate. Additionally, sexually transmitted infections (STIs) may contribute to the development of this condition. Another potential risk factor is a history of medical procedures involving the prostate, such as biopsies or surgeries. These interventions can introduce foreign materials or cause tissue damage, provoking an inflammatory response that results in granuloma formation. Furthermore, certain medications and treatments, including Bacillus Calmette-Guerin (BCG) therapy for bladder cancer, have been associated with granulomatous prostatitis. Genetic predisposition may also influence the likelihood of developing granulomatous prostatitis. Individuals with a family history of autoimmune diseases or other inflammatory conditions may be at greater risk. Additionally, environmental factors and lifestyle choices, such as smoking or exposure to certain toxins, might contribute to the development of this condition. Understanding these causes and risk factors is crucial for both patients and healthcare providers. By recognizing the potential triggers and underlying mechanisms, appropriate diagnostic and therapeutic approaches can be employed to manage granulomatous prostatitis effectively.
Diagnosis of Granulomatous Prostatitis
The diagnosis of granulomatous prostatitis is a multifaceted process that typically involves a combination of clinical evaluation, radiological imaging, and histopathological examination. Initially, a detailed patient history and physical examination are essential. Symptoms such as urinary retention, painful urination, and pelvic discomfort often prompt further investigation. Laboratory tests, including blood tests and urinalysis, may be conducted to rule out infections and other conditions. Prostate-specific antigen (PSA) levels are also measured, although they can be elevated in both granulomatous prostatitis and prostate cancer, thus complicating the diagnostic process. Therefore, imaging studies like transrectal ultrasound (TRUS) and magnetic resonance imaging (MRI) are frequently employed. These imaging techniques can help identify abnormalities in the prostate but are not definitive for diagnosing granulomatous prostatitis. The gold standard for a conclusive diagnosis is a prostate biopsy. During this procedure, tissue samples from the prostate are obtained and examined under a microscope. The presence of granulomas—an accumulation of macrophages, giant cells, and other immune cells—confirms the diagnosis of granulomatous prostatitis. It’s important to note that the biopsy not only helps in diagnosing the condition but also rules out malignancies such as prostate cancer, which can present with similar clinical features. Once a diagnosis of granulomatous prostatitis is established, tailored treatment plans can be formulated to manage the symptoms and underlying causes effectively.
Treatment Options for Granulomatous Prostatitis
When it comes to treating granulomatous prostatitis, the approach can vary based on the underlying cause of the condition. It is essential for healthcare providers to identify whether the granulomatous inflammation is due to an infection, an autoimmune response, or another factor. Here are some common treatment options for managing granulomatous prostatitis: 1. **Antibiotics:** If the granulomatous prostatitis is suspected to be caused by a bacterial infection, a course of antibiotics may be prescribed. It is crucial to complete the entire course of antibiotics to ensure the infection is fully eradicated. 2. **Anti-inflammatory Medications:** Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be used to reduce inflammation and alleviate pain associated with granulomatous prostatitis. These medications can help manage symptoms and improve the patient’s quality of life. 3. **Observation and Monitoring:** In some cases, especially when the granulomatous inflammation is mild and asymptomatic, a ‘watchful waiting’ approach may be adopted. Regular monitoring and follow-up appointments are necessary to ensure the condition does not worsen or lead to complications. 4. **Immunosuppressive Therapy:** For cases of granulomatous prostatitis linked to autoimmune responses, immunosuppressive drugs may be prescribed. These medications help to modulate the immune system and minimize the inflammatory response within the prostate. 5. **Surgical Intervention:** In rare and severe cases where granulomatous prostatitis leads to significant obstruction or other complications, surgical procedures such as transurethral resection of the prostate (TURP) may be considered. Surgical intervention is typically a last resort when other treatments have failed. 6. **Lifestyle Modifications:** Patients may also benefit from making certain lifestyle changes, such as adopting a healthy diet, increasing physical activity, and avoiding irritants like caffeine and alcohol. These modifications can help manage symptoms and support overall prostate health. Every patient’s situation is unique, and therefore, treatment plans should be tailored to the individual’s specific needs and the underlying cause of the granulomatous prostatitis. Collaboration between urologists, primary care physicians, and other healthcare providers is essential to ensure comprehensive care and effective management of this complex condition.
Potential Complications
Granulomatous prostatitis có thể dẫn đến một loạt các biến chứng tiềm ẩn, đòi hỏi sự theo dõi và can thiệp y tế kịp thời để quản lý hiệu quả. Một trong những biến chứng phổ biến là sự hình thành các u hạt lớn gây chèn ép niệu đạo hoặc cổ bàng quang, dẫn đến các vấn đề về tiểu tiện như tiểu khó, tiểu buốt, hoặc cảm giác tiểu không hết. Các triệu chứng này có thể ảnh hưởng đáng kể đến chất lượng cuộc sống và đòi hỏi can thiệp y tế để giảm bớt áp lực lên đường tiểu.\n\nMột tiềm năng nghiêm trọng khác là sự nhầm lẫn giữa granulomatous prostatitis và ung thư tuyến tiền liệt. Các u hạt trong tuyến tiền liệt có thể gây ra hình ảnh tương tự với ung thư khi kiểm tra bằng các phương pháp hình ảnh y tế như siêu âm hoặc MRI. Điều này có thể dẫn đến các sinh thiết không cần thiết hoặc thậm chí là các can thiệp phẫu thuật không cần thiết, gây ra tâm lý lo lắng và thậm chí là các biến chứng sau phẫu thuật.\n\nViệc điều trị không đầy đủ hoặc không phù hợp của granulomatous prostatitis cũng có thể dẫn đến các biến chứng như nhiễm khuẩn kéo dài hoặc tái phát nhiễm khuẩn. Các đợt viêm kéo dài có thể làm tổn thương mô tuyến tiền liệt và dẫn đến viêm mãn tính, gây ra sự khó chịu lâu dài và ảnh hưởng xấu đến chức năng sinh dục và hệ tiết niệu.\n\nDo đó, việc nhận diện và quản lý đúng đắn các biến chứng của granulomatous prostatitis là vô cùng quan trọng. Các bác sĩ cần phải cẩn trọng khi chẩn đoán để tránh nhầm lẫn với ung thư tuyến tiền liệt và chọn ra phương pháp điều trị phù hợp nhằm giảm thiểu các biến chứng và cải thiện chất lượng cuộc sống cho bệnh nhân.
Living with Granulomatous Prostatitis
### Living with Granulomatous Prostatitis Living with granulomatous prostatitis can be challenging due to the chronic and often unpredictable nature of the condition. Individuals diagnosed with this type of prostatitis may experience persistent pain, discomfort, and urinary symptoms that can significantly impact their quality of life. Daily activities, including urination, sexual function, and even sitting for extended periods, can become difficult to manage. One of the key aspects of living with granulomatous prostatitis is understanding how to manage the symptoms effectively. Pain management is crucial and can involve a combination of medications, lifestyle changes, and alternative therapies. Regular consultations with healthcare professionals, such as urologists or pain specialists, can help tailor a treatment plan that addresses the specific needs of the individual. Incorporating lifestyle modifications can also play a significant role in alleviating symptoms. Staying hydrated, maintaining a balanced diet, and engaging in moderate physical activity can improve overall health and potentially reduce the severity of symptoms. Additionally, avoiding irritants such as caffeine, alcohol, and spicy foods may help minimize discomfort during flare-ups. Mental health is another critical aspect of living with granulomatous prostatitis. Chronic illnesses can lead to feelings of frustration, anxiety, and depression. Seeking support from mental health professionals, joining support groups, or connecting with others who have similar experiences can provide emotional relief and coping strategies. Living with granulomatous prostatitis requires a proactive approach to symptom management and a strong support network. With the right strategies and support, individuals can navigate the challenges of this condition and lead fulfilling lives.